Member Q&A: Meet new center member Dr. Ranmal Samarasinghe
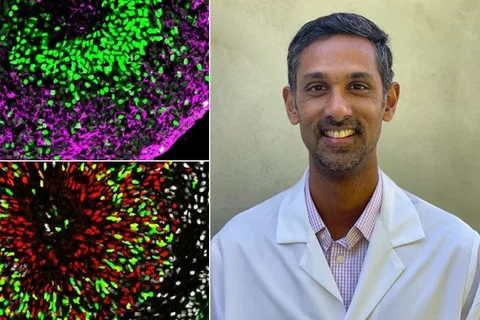
As an assistant professor of neurology at the David Geffen School of Medicine, Dr. Ranmal Samarasinghe’sresearch focuses on how neurons connect to form neural circuits in the brain and how circuit dysfunction is associated with diseases like epilepsy and autism. Prior to becoming a UCLA faculty member and opening his own lab, Samarasinghe trained in the lab of UCLA Broad Stem Cell Research Center member Bennett Novitch, Ph.D. He and Novitch continue to collaborate using brain organoids – simplified three-dimensional human brain tissue grown from stem cells – to study how epilepsy impacts the brain’s rhythms.
Samarasinghe discussed why epilepsy can be difficult to treat, how brain organoids can help scientists better understand neurological disorders and his experience as a clinical fellow in the center’s stem cell training program.
This interview had been edited for clarity
What attracted you to the brain as an area of study?
When I was much younger, I remember asking the question, ‘what makes me me?’ And the answer, to me at least, is the brain; it’s the seat of consciousness. I was in the third or fourth grade and it was one of those things that was kind of weird to think about, but stuck with me throughout my education. And then, when I had to decide on a career path, neuroscience and neurology seemed like a natural fit. They related to what I asked myself all those years ago, never really being able to answer that question, but thinking that studying the brain is how I might get closer to an answer.
Why is epilepsy such a difficult condition to treat?
One important answer is that we don’t really understand the precise changes in the brain that result in epilepsy. Epilepsy is not one disease. Epilepsy is many, many diseases and so there are certain epilepsies that we are actually very good at treating. You give a single medication and the patient does well, for example, and doesn't have another seizure in their life. And then there are other epilepsies that we’re not currently successful at treating. It’s a spectrum and we use the term epilepsy to describe all of this, but not every type of epilepsy is the same. What is the same about them is that you can see similar symptoms, but what happens in the brain to produce those symptoms can be very different. We have much less of an understanding about why those neural networks or why those pathological events happen in the brain to produce that condition. And so, if you don't fully understand the underlying cause, treating the disease is difficult.
Why are new treatments for epilepsy needed?
So, in adults, we can effectively treat about 70% of epilepsy patients with medications, but 30% of patients are not responsive to medications. That statistic hasn't changed in essentially 100 years even though we've added a whole bunch of new medications over the last 30 to 40 years. From those new medications, we've gained some improvement in side effects certainly and some modest improvement in what we can treat and how we can treat it.
But beyond that, in terms of achieving seizure freedom in the case of epilepsy, going from multiple epileptic seizures down to zero, we've hit roadblocks. Part of it is a lack of understanding around the neurological processes that underlie human epilepsy and another part of it is the need for more detailed and complementary disease modeling.
In the case of modeling, one problem is that drugs that may work well in a rodent model may not work in a human. So we can be successfully curing seizures in animals. But, you know, if you're curing epilepsy in a mouse, you're curing epilepsy in a mouse and not a human. And the idea is we want to cure a human, so the new brain organoid models and the physiological data they unlock will hopefully become important tools to move us towards that goal in tandem with the ongoing work in animal models, which must also continue. These systems will likely be complementary and together hopefully paint a more complete picture of the disease process.
How do the patients you see in the clinic inspire your research?
I see adult patients mostly, but I've been seeing more pediatric patients recently because it's so much more relevant to my research. The patients themselves are sometimes severely devastated by their epilepsy and, of course, all of us involved in their care want to do more. But in some ways, what really strikes me is what their parents have to go through because it’s so relatable to me personally. I'm a parent of two young kids and I see what my patients’ parents have to go through and I am very inspired by the kind of sacrifices that, almost without exception, all of these parents make to take care of their children. It's unbelievable. For some of these patients, the parents have to perform the care that I need to give to my younger kid who is 18 months old, but they have to provide this level of care for the rest of their children’s lives, essentially, and more - a lot more.
So the inspiration is driven partly out of wanting to help the patients, but importantly in my case, also by the effect of the disease on families because it personally relates to me as a parent with young kids.
How do stem cell-derived brain organoids help researchers better understand and discover new treatments for epilepsy and other neurological disorders?
The idea is to try to understand how neural circuits, which means the interaction between neurons within that brain organoid, are normal or abnormal in disease states versus non-disease states. That functional circuit in the brain is required to generate a brain rhythm, like those seen in an EEG. EEG tests measure the electrical patterns that occur in the brain when one part of the brain communicates with another.
For example, in certain disease states, EEG rhythms are different. And that's how we utilize EEGs- like a healthy patient has a certain pattern, certain states of disease or ‘brain unhealth,’ are associated with different EEG patterns. To take that to the next level in terms of organoids, we've developed techniques to actually see these kinds of rhythms, these brain rhythms, within organoids. And so now the next question is, what interactions between cells and what kinds of cells are important to generate these rhythms? When they're not present, why is that? What is it about the disease that changes the formation of these units, circuits, networks -whatever you want to call it- so that we don't see the rhythm?
In terms of treatments specifically, understanding causes of diseases is, of course, an important step towards treatment. But, in addition, we can also potentially use the organoid as a tool to test drugs in the dish. For example, we can generate a number of organoids using induced pluripotent stem cells derived from the skin cells of a particular patient with an incurable epilepsy, measure the abnormal ‘brain waves’ in these organoids and then identify and test drugs that may normalize the brain waves. These drugs can then potentially be of value in the clinic.
Can you describe your experience in the center’s stem cell training program?
It was nice, first of all, to see some of the other work that was happening and to be involved in the stem cell center’s community in a formal way. UCLA is a big place and it's easy to not get involved and not become a part of the community that you should naturally be a part of. As someone who was seeking to be independent, I could have just been in Ben’s [Novitch] lab focused on Ben’s stuff, but it shouldn’t be overlooked how important it is to branch out.
And then there was the idea that you need to be able to talk about your research in a way that's accessible. And there was an emphasis on that, which I think many of us [scientists] don't think about because we spend our days talking to people who know what we're talking about.
Why is funding for training programs like the one you participated in important to the future of science?
The value is two-fold. One is providing financial support allows us to do what we want to do. The second is some of the formal things, like practice with writing and submitting grants, formal scientific talks, and giving shorter presentations geared to a lay audience.
Getting practice and guidance with presentations to a lay audience was an especially unique and helpful aspect of the training program. There was an emphasis on learning how to talk about your research in an accessible way, giving that elevator speech, for example, like that's a really important skill, and whether I am able to do it well now or not, at least I learned to think about it.
[Editor’s note: Samarasinghe is being overly modest. You can watch this recording of a presentation he gave in January 2021 to see his excellent science communication skills in action]
Original Article: "Member Q&A: Meet new center member Dr. Ranmal Samarasinghe"



