UCLA researchers engineer resistance-proof CAR T cells
In a Phase 1 clinical trial, the ‘bispecific’ therapy showed safe, long-lasting results
In the six years following the approval of the first-ever chimeric antigen receptor (CAR) T-cell therapy in 2017, the treatment has saved lives and revolutionized cancer care.
UCLA Health has been an integral part of the immunotherapy revolution. In 2018, it became one of the first health systems in the country to offer commercial CAR T-cell therapy and launched a formal program (PDF) that same year.
Now, UCLA scientists who are at the forefront of CAR T-cell research are working to make the therapy safer, more effective, and more accessible for a greater number of patients, says Sarah Larson, MD, an associate clinical professor of medicine at the David Geffen School of Medicine at UCLA, a hematology and oncology specialist at UCLA Health and a UCLA Jonsson Comprehensive Cancer Center member.
“UCLA is one of the few medical sites where we can develop our own CAR T cells,” Dr. Larson says. “We have all of the FDA-approved products available for patients, we have clinical trials, including investigator-initiated trials that are not just in partnership with industry, but are fully home-grown, which is really unique.”
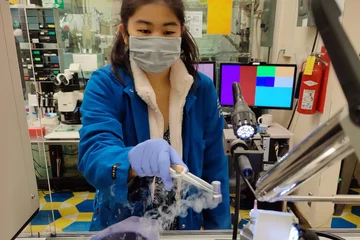
A form of gene therapy, CAR T-cell treatments harness a patient’s own immune system to kill cancer. Treatment starts by collecting a patient’s T-cells — a type of white blood cell that protects the body from infection — through an IV.
The patient’s immune system cells are then sent to a lab where researchers modify them with a gene for a chimeric antigen receptor, or CAR, which is able to bind to tumor-specific proteins on the surface of cancer cells. This allows the modified T-cells to find and kill cancer.
The CAR T cells are then multiplied by millions in the lab, shipped back to the hospital, and infused into the patient via an IV drip.
Overcoming challenges
Tisagenlecleucel (brand name Kymriah) became the first CAR T-cell therapy approved by the Food and Drug Administration (FDA) to treat B-cell acute lymphoblastic leukemia (ALL) in 2017. Since then, the FDA has approved five other CAR T-cell therapies. All are approved for the treatment of blood cancers, including lymphomas, multiple myeloma, and some forms of leukemia.
Still, challenges persist.
One serious side effect of CAR T-cell therapy is that the modified immune cells can overload the bloodstream with cytokines. Cytokines help moderate inflammation, and an overload can lead to high fevers and drops in blood pressure — a response called cytokine release syndrome (CRS). Because of the high risk of CRS, many patients require the concurrent use of the immunosuppressant drug tocilizumab (Actemra) while on CAR T-cell therapy.
The treatment can also lead to immune effector cell-associated neurotoxicity syndrome (ICANS), which occurs when cytokines disrupt the blood-brain barrier. It can be deadly.
Moreover, patients can develop resistance to CAR T-cell therapy once the modified immune cells lose either some or all of their target antigen expression — a phenomenon called antigen escape. “It’s one of the major ways that patients relapse,” Dr. Larson says.
To overcome this, Yvonne Chen, PhD, associate professor of microbiology, immunology, and molecular genetics, has designed a type of “bispecific” CAR that can recognize two different tumor markers in patients with non-Hodgkin’s lymphoma: CD19 and CD20. By targeting two different antigens, the risk of antigen escape is lowered, and patients remain in remission longer.
In a Phase 1, first-in-human clinical trial led by Dr. Chen and Dr. Larson, researchers treated 11 patients with relapsed/refractory non-Hodgkin’s lymphoma with autologous-naive and memory T cells engineered to express a bispecific anti-CD19/CD20 CAR.
As of March 2023, 10 of the 11 patients responded to the treatment, and eight of 11 achieved a complete response, according to findings presented at the American Association for Cancer Research annual meeting. The median progression-free survival was 18.2 months.
“With such a small number of patients, a 73% response rate is really impressive,” Dr. Larson says.
But what was most promising for Dr. Larson and the research team was just how safe the treatment turned out to be. Zero of the patients experienced neurotoxicity, and only one patient required treatment for CRS. Dr. Larson says that the therapy’s lack of side effects, despite its strong potency, may be related to the CARs' ability to “debulk,” or reduce, the tumor cells early before there is an overwhelming cytokine response.
The trial is ongoing. This month, the FDA granted a Fast Track Designation for the therapy, which means that the drug could receive accelerated approval. The UCLA-led research team is also in the process of developing a dual target CAR-T treatment for patients with multiple myeloma.
Dr. Larson says that the high efficacy and safety of the new treatment could allow medical centers to administer it in an outpatient setting, and patients would not need to take tocilizumab, the immunosuppressing drug.
“Having this kind of a safety signal really opens up accessibility to patients and more comfort for providers who have less experience with CAR T cells,” she says.
She adds that as research continues, the field will find solutions to other challenges, such as how to use CAR T cells in solid tumors and how to make the treatment more widely available and cost-effective for patients outside of academic health systems.