Endometriosis Symptoms, Treatment, and Causes
Medical Expert Interview

“This disease affects someone you know. And it is ruining her life. And it doesn't have to. There is help.”
In this article:
- Endometriosis Definition
- Endometriosis Causes
- Endometriosis Symptoms
- Endometriosis Diagnosis
- Endometriosis Stages
- Endometriosis Treatment
Meet Dr. Daniel N. Ginn
A Clinical Instructor of UCLA Obstetrics and Gynecology, Dr. Ginn decided to specialize in the treatment of endometriosis when he was in his senior year of residency. As a chief resident, he was frustrated by the way patients with pelvic pain were usually handled, even by the best doctors.
“We were not sufficiently addressing what a lot of patients brought to the table,” recounts Dr. Ginn. “And that just never sat well with me.”

He’s now passionately committed to making a difference for those suffering from chronic pelvic pain, including patients who have endometriosis.
“It breaks my heart,” he confesses. “I cry with patients in clinic because so many of them have been through so much already. And they've been gas lit, either intentionally or otherwise. Told that they're exaggerating their symptoms, or they're too weak, or they're not strong enough, or something like that.”
Dr. Ginn takes a decidedly different approach.
“The way that you actually help somebody is having the patience and the willingness to dig in with them. To understand the specific components of their problem.”
In honor of Endometriosis Awareness Month, Dr. Ginn shares his thoughts on the best way to identify endometriosis symptoms as well as using the right tools to support a diagnosis. He also talks about various treatment options, common misconceptions about the disease, and where he thinks there’s room for improvement.
(What Is a Gynecologist? Click the link to learn more...)
What Is Endometriosis?
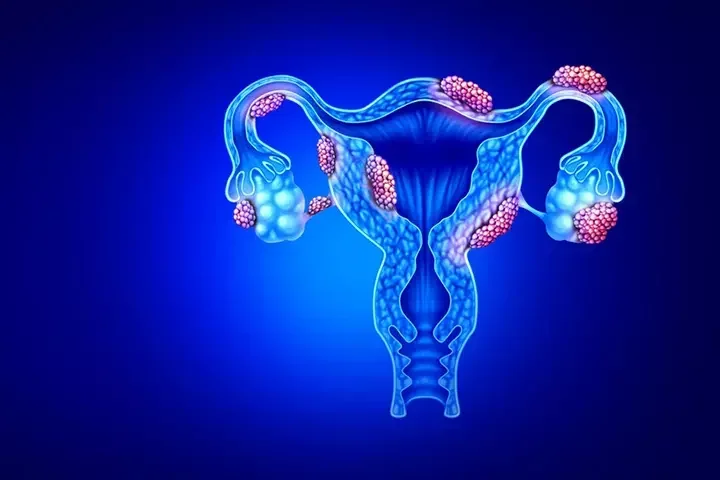
Endometriosis is a medical condition that occurs when the tissue that normally lines the inside of the uterus starts to grow outside of the uterus, usually on other organs in the pelvic area such as the ovaries, fallopian tubes, or lining of the pelvis. In some cases, however, it can even affect areas outside the pelvic cavity, such as the diaphragm or lungs.
This tissue can still thicken and break down like it does inside the uterus during the menstrual cycle. But because it has no way to exit the body, it can lead to inflammation, scarring, and pain.
How Common Is Endometriosis?
Endometriosis is a relatively common condition, affecting an estimated 6-10% of individuals with female reproductive organs during their reproductive years (usually between the ages of 15 and 49).
What Causes Endometriosis
The causes of endometriosis are not fully understood, but there are several theories.
One theory is that during menstruation, some of the menstrual blood containing endometrial cells flows backwards through the fallopian tubes and into the pelvic cavity. Then it implants and grows on other organs. This is known as retrograde menstruation.
However, as Dr. Ginn notes, retrograde menstruation is actually a common phenomenon while endometriosis only affects 6-10% of the female population. “If we see retrograde menstruation in everybody, then we should see endometriosis in everybody. But we don’t.”
Other theories suggest that endometrial cells may spread through the bloodstream or lymphatic system (called “extrapelvic endometriosis”). Or that they may be present outside of the uterus from birth due to embryonic development (called “müllerianosis”).
Other possible endometriosis causes include an inherent dysfunction of the peritoneal immune system or even coelomic metaplasia. “That’s just a fancy way of saying that some of the cells lining the peritoneum change into the wrong kind of tissue,” explains Dr. Ginn.
Is Endometriosis Genetic? Is Endometriosis Hereditary?
There is evidence to suggest that endometriosis may have a genetic component, meaning that it can be inherited from one's parents. Studies have found that women who have a first-degree relative (such as a mother or sister) with endometriosis are 7-10 times more likely to develop the condition.
However, it is important to note that genetics alone do not determine whether or not an individual will develop endometriosis. Other factors such as hormonal imbalances, immune system dysfunction, and environmental exposures may also play a role in the development of the condition.
It is likely that endometriosis is caused by a combination of these and other factors. And researchers are still working to better understand the underlying mechanisms of the condition.
What Does Endometriosis Feel Like? What Are the Symptoms of Endometriosis?
Endometriosis can cause a range of symptoms, and the experience can vary widely among individuals. Some people may have no symptoms at all, while others may experience severe pain and discomfort.
The most common symptoms of endometriosis include:
- Pelvic Mass: Also called an “adnexal mass,” this growth occurs in or near the uterus, ovaries, fallopian tubes, and the connecting tissues.
- Infertility: Endometriosis can affect fertility by causing damage to the reproductive organs or blocking the fallopian tubes.
- Painful Periods (Dysmenorrhea): Endometriosis can cause menstrual cramps that are more severe than usual. And the pain may begin several days before the period starts and continue for several days after.
But what is considered normal when it comes to menstrual cramps? That’s a loaded question, according to Dr. Ginn.
“So many patients come from families where everybody's periods are really bad. And they grow up thinking that is normal because it was normal in their family. Only to be told by somebody like me, it was never normal. And they’ve missed years of opportunities to intervene.”
So where should a patient draw the line between normal and abnormal menstrual pain? “If they’re not getting relief with Ibuprofen or Tylenol and they're missing out on their life—they're missing school or calling in sick to work—that's not normal,” says Dr. Ginn.
Additional symptoms of endometriosis include:
- Non-Menstrual Pelvic Pain: The pain may be felt in the lower abdomen, pelvis, or lower back, and can range from mild to severe.
- Painful Intercourse (Dyspareunia): Endometriosis can make sexual intercourse painful or uncomfortable, especially during deep penetration.
- Digestive Issues: In some cases, endometriosis can cause gastrointestinal symptoms such as vomiting, bloating, constipation, or diarrhea, especially during menstruation. It can also be associated with painful bowel movements (dyschezia).
- Painful Bladder or Urination (Dysuria): If endometriosis affects the bladder or urethra, symptoms can include pain when the bladder is full, burning or pain during urination, and an urgent or frequent need to urinate.
Less common symptoms include:
- Chest Pain: In rare cases, endometrial tissue can grow on the diaphragm, lungs, or other parts of the chest cavity. This can cause chest pain, shortness of breath, or even referred pain to the shoulder.
- Allergies or Sensitivities: Endometriosis may cause an immune system response, leading to allergies or sensitivities to certain foods or environmental factors.
However, as Dr. Ginn notes, these symptoms can also be caused by other conditions, so a proper medical evaluation is necessary to determine the cause. “For many patients with chronic pelvic pain there is almost never one diagnosis that explains all of their symptoms.”
And effectively diagnosing and treating endometriosis requires a thorough approach. “A lot of patients have these overlapping symptoms you have to tease apart to be able to help people actually make improvement and get better,” explains Dr. Ginn. He often tells his patients: “You told me you had one problem. I hear four problems, and if we don't make a plan for all four problems, you're not going to get better.”
What Is Endometriosis Confused With? Which Conditions Have Similar Symptoms?
- Benign Ovarian Cysts
- Adenomyosis
- IBS or Irritable Bowel Syndrome
- Adhesions
- Neuropathic Pain
- Pelvic Floor Disorders
- Hemorrhoids
- Interstitial Cystitis
- Anal Fissures
Does Endometriosis Cause Weight Gain?
Endometriosis itself does not directly cause weight gain. However, some individuals with endometriosis may experience weight gain as a result of the condition or its treatment. For example, chronic endometriosis pain can make it difficult to maintain an active lifestyle. And reduced physical activity can lead to weight gain. Additionally, hormonal treatments used to manage endometriosis, such as birth control pills, can cause weight gain as a side effect.
Can Endometriosis Cause Back Pain?
Back pain is a common symptom of endometriosis, particularly in the lower back and pelvic area. The pain may be described as a dull ache or sharp, stabbing pain. And may be worse during menstruation or during sexual activity. This happens when endometrial tissue implants on the ligaments and muscles in the pelvic area, which can cause tension and pain in the lower back. Additionally, endometriosis can cause inflammation in the pelvic area, which can also contribute to back pain.
What Is Endometriosis Belly?
Endometriosis belly is a term used to describe a distended or swollen abdomen that may be caused by endometriosis. The condition can cause a buildup of tissue and fluid, which can lead to bloating and abdominal discomfort. Endometriosis belly can also be a result of hormonal changes and inflammation associated with the condition.
What Is an Endometriosis Cyst?
Also known as an endometrioma or chocolate cyst, endometriosis cysts are formed when endometrial tissue grows on the ovaries and forms a fluid-filled sac. The fluid inside the sac may look dark and thick, like chocolate. These cysts can cause a range of symptoms, including pelvic pain, abdominal bloating, irregular periods, and painful periods. In some cases, endometriomas can also interfere with fertility.
How to Diagnose Endometriosis
In short, there are four steps to an endometriosis diagnosis:
1. Medical History
Doing a thorough and careful medical history is absolutely crucial when endometriosis is suspected. Healthcare providers should ask questions about the patient’s symptoms, menstrual cycle, and medical history, including any family history of endometriosis.
Dr. Ginn asks the same eight questions during his screening process:
- Do you have a period every month?
- How many days do you bleed?
- How many days are heavy?
- How fast do you soak up pad or tampon at the heaviest bleeding?
- Do you have pain with your period?
- Do you have pain with intercourse?
- Do you have other pelvic pain?
- Do you leak urine?
“That short series of questions tells me if someone has abnormal bleeding, heavy bleeding, painful periods, pain with sex, or urine leakage,” says Dr. Ginn. “And then I can tailor a management plan really quickly based off of that.”
2. Physical Exam
A pelvic exam should be performed to check for any abnormalities or signs of endometriosis.
3. Imaging Tests
Imaging tests, such as ultrasound or magnetic resonance imaging (MRI), may be used to detect the presence of endometrial tissue and any associated complications, such as cysts or scarring.
According to Dr. Ginn, this is a key step in the diagnostic process, and one that’s often misunderstood because there’s a big difference between a “routine” ultrasound and a “specialty protocol ultrasound” which is designed specifically to check for endometriosis. “Sending a patient for a routine ultrasound is the wrong thing to do.”
4. Laparoscopy
Laparoscopy is a minimally invasive surgical procedure that allows a healthcare provider to examine the pelvic area and remove tissue samples for biopsy.
At present, the average age at diagnosis is 28 years old. However, that’s not necessarily because patients don’t exhibit or experience symptoms earlier. “The reason the average age of diagnosis is so late is because it can take 7-9 years to get to a diagnosis on account of trying other things first,” posits Dr. Ginn. “By the time patients make it to me, I'm usually like the fifth to tenth doctor that they've seen.”
Endometriosis Stages
The stages of endometriosis are based on the location, extent, and severity of the endometrial tissue growth, as well as the presence of adhesions or scar tissue. The four stages of endometriosis are:
- Stage 1 (minimal): In stage 1, there are small patches or isolated implants of endometrial tissue outside the uterus. There may be some inflammation but no significant scar tissue or adhesions.
- Stage 2 (mild): In stage 2, there are more widespread implants of endometrial tissue. And there may be some small cysts or endometriomas. There may also be some mild adhesions or scar tissue.
- Stage 3 (moderate): In stage 3, there are multiple implants of endometrial tissue, some of which may be deep and involve organs outside the uterus. There may be significant adhesions and scar tissue, and there may be the formation of large endometriomas.
- Stage 4 (severe): In stage 4, there are extensive implants of endometrial tissue, including deep infiltration into organs outside the uterus. There may be large endometriomas, significant adhesions and scar tissue, and distortion or blockage of the pelvic anatomy.
It's important to note that the severity of endometriosis does not necessarily correspond to the severity of symptoms. Some individuals with mild endometriosis may experience severe pain and other symptoms, while others with severe endometriosis may have few or no symptoms at all.
“Most people have some symptoms that more or less track to their severity of disease,” says Dr. Ginn. “But, yes, it's possible to have the disease and not know it. One person’s stage 1 finding is someone else’s stage 4 symptom. Someone else’s stage 4 findings are someone else’s stage 2 symptoms.”
What matters most, he insists, is tackling each case with a personalized approach.
“In the end, we treat the patient as an individual.”
How to Treat Endometriosis
There are several treatments available for endometriosis. The appropriate choice will depend on the severity of the symptoms, the extent of the endometrial tissue, and other individual factors such as age and desire for future pregnancy. “We have to understand what the patient’s goals are,” maintains Dr. Ginn. “For example, most of the medical management options for endometriosis are counterproductive to trying to get pregnant.”
Some common treatments for endometriosis include:
Medical Management
Hormone therapy—such as birth control pills, progestin-only pills, or gonadotropin-releasing hormone (GnRH) agonists and antagonists—can help regulate or inhibit the menstrual cycle as well as halt or reduce the growth of new endometrial tissue.
“If you can stop the period, then you may stop the pain,” explains Dr. Ginn. “And we can usually do that with manipulation of routine, hormonal contraceptives. So pills, patches, rings, IUDs, or birth control pills can be taken with an extended cycle where they have a period every 3 or 4 months. Or they can be taken continuously, intending to have a period never.”
However, Dr. Ginn warns that patients taking endometriosis medication can experience side effects including: breakthrough bleeding, hair loss, nausea, mood changes, weight gain, hot flashes, and decreased bone density.
This is especially true of GnRH agonists and antagonists, which Dr. Ginn does not recommend taking long term. “I view those medications as a band aid,” he admits. “They're great for somebody who's really close to menopause that might see their estrogen levels dropping and their symptoms improving. Or they might be good for someone who is just trying to buy time because they're in school and they can't take time off for surgery until the summer.”
Endometriosis Surgery
In some cases, surgery may be necessary to remove endometrial lesions and scar tissue. This may be done through laparoscopy, a minimally invasive surgical procedure that allows examination of and access to the pelvic area.
In more severe cases, a healthcare provider might recommend a hysterectomy for endometriosis. This may be necessary to remove all disease and may also be recommended in patients with adenomyosis who do not desire future fertility or those with abnormal bleeding that is not responsive to medication.
“Surgery should be considered,” says Dr. Ginn. “Especially if a patient has tried medical management and had limited, short-term or no improvement in their symptoms.”
How soon after starting medication should the idea of surgery be introduced? “If someone goes through one or two different trials of conservative therapy over a set period of time, maybe 3 months, and if we don't make progress, then we're making a new decision,” insists Dr. Ginn.
There are, however, reasons to consider surgery even sooner. “If you find a large cyst on the ovary that you're worried is going to get twisted on itself, if someone has evidence of tubal blockage and they're trying to get pregnant, if they have lesions that are invading their bowels or bladder or obstructing the ureter, they need surgery earlier.”
Alternative Therapies
Some individuals may find relief from endometriosis symptoms through alternative treatments such as dietary changes or pelvic floor physical therapy.
In fact, Dr. Ginn contends that many endometriosis patients—especially those who have been dealing with symptoms of the disease for years—could probably benefit from pelvic floor PT. “All the time I send people to physical therapy who should have gone five years ago.”
Overall, the most important part of an endometriosis treatment plan is understanding that every patient’s experience is unique. “Somebody who has really painful periods but also has heavy bleeding might need slightly different management than someone who's only got pain or only has heavy bleeding,” explains Dr. Ginn.
And the right treatment plan may very well involve seeing additional specialists. “If the patient has symptoms that are GI oriented, possibly IBS, then they need to see a gastroenterologist,” says Dr. Ginn. “If patients have pain with their urination, then they may need to see a urologist. If the patient has pain with sexual intercourse, then we need to get them into pelvic physical therapy. Because that won't get better with medication, and it won't get better with surgery either.”
While there is no endometriosis cure, these treatments can help manage symptoms and improve a patient’s quality of life.
Can You Get Pregnant With Endometriosis? Does Endometriosis Cause Infertility?
Yes, it is possible to get pregnant with endometriosis. But it may be more difficult for some individuals due to the effect of endometriosis on fertility.
“The real answer is we don’t understand this relationship that well,” reveals Dr. Ginn. “Other than knowing that it occurs.”
So what are the potential connections between endometriosis and fertility?
Endometriosis can cause the formation of scar tissue and adhesions that can block or damage the fallopian tubes. That makes it more difficult for the egg and sperm to meet. In addition, endometriosis can diminish the ovarian reserve and reduce the chances of implantation in the uterus (possibly due to adenomyosis). Plus, inflammation caused by endometriosis can damage the sperm as well as the eggs.
However, many individuals with endometriosis are still able to conceive naturally or with the help of fertility treatments. In fact, some women with endometriosis may not even be aware that they have the condition until they have difficulty getting pregnant.
Setting the Record Straight: Common Misconceptions
Dr. Ginn says there are three main misconceptions he wants to see addressed:
1. That cyclic birth control is appropriate management.
“What I tell people is that your grandmother was mostly right: if you're not on birth control, you need to have a period every month,” says Dr. Ginn. But patients on hormone management can safely skip their monthly menstruation, and it’s definitely something to consider if period cramps are abnormally painful. “If your periods are disruptive to your life because of bleeding, pain, or both, having a period of less frequently (or never) is a safe option. For a lot of people, that might be all they need to do.”
2. That it's normal to miss school or work because of period pain.
Many patients with endometriosis have had symptoms for many years but didn’t realize it because they didn’t have a clear understanding of what normal menstrual periods look like. “They should be able to take Ibuprofen and go to dinner, or take Ibuprofen and go to school,” says Dr. Ginn. “That's ‘normal’ menstrual cramps.”
3. That there's nothing that can be done.
“I think that's probably the biggest one, is that they can't be helped,” says Dr. Ginn. “They can. They can be helped.” And it’s important that patients who think they might have the disease seek medical care. “Endometriosis—while it's not malignant like cancer—it can damage organs in a way that can be life-threatening if they don't do anything about it.”
Looking Forward: What Needs to Change
Dr. Ginn has several thoughts about things we can focus on improving when it comes to endometriosis:
1. Talking about pain.
According to Dr. Ginn, period pain should be moderate and controllable: “Anything more than that needs more work up.” However, this telltale sign of endometriosis is often overlooked because people—patients, parents, teachers, and even doctors—either don’t want to or know how to talk about pain.
“Nobody wants to ask about pain because it's a Pandora's box,” he laments. Even doctors often skip this question but it’s a critical aspect of patient care.
And he’d like to see school nurses get more involved, guiding parents who might not realize their child needs help. If a student consistently misses class due to painful period cramps, then it’s time to see a specialist.
2. Using appropriate diagnostic imaging.
It’s frustrating that many women seek diagnosis and treatment for their symptoms but are mistakenly told by their healthcare provider that everything is fine because the right diagnostic tools weren’t used.
“Many patients with a history of endometriosis have been told they had a normal or negative ultrasound and therefore couldn’t have endometriosis,” says Dr. Ginn. “And that’s not true.”
Dr. Ginn wants everyone—both patients and providers—to understand how to test for endometriosis. The key here is utilizing a “specialty protocol ultrasound” designed to uncover endometriosis. A routine ultrasound is the wrong approach.
An MRI can also help during the diagnostic process, especially if the specialty protocol ultrasound reveals nothing but the symptoms are very convincing.
It is important to note that even specialty protocol imaging is not perfect and does not definitively rule out endometriosis. Very small lesions still may not be visible.
"Imaging is our guide," explains Dr. Ginn. "But we still have to correlate symptoms. And if symptoms are not supported by imaging, but suspicion of the disease is high, we still need to consider surgery, especially if conservative medical management is not effective."
3. Providing quality pelvic floor physical therapy.
This is a critical yet often overlooked treatment for endometriosis and chronic pelvic pain. And Dr. Ginn believes it should be available to anyone with a pelvic floor disorder, whether it’s caused by endometriosis, childbirth, or something else. Unfortunately, many patients don’t even realize they need this treatment because their healthcare provider missed it during the diagnostic process.
“If you don't ask the right questions for it and you don't do the exam, you will miss the diagnosis every time,” says Dr. Ginn. “And it’s easy to catch, which is disappointing.”
4. Increasing access to proper care.
One of the reasons Dr. Ginn chose UCLA was because it provided an opportunity to be part of a team tasked with building a formal, multi-disciplinary program for the treatment of endometriosis and chronic pelvic pain, something every woman should have access to. That’s often a challenge, however, for many patients. “That's the really hard part for people who live in smaller communities that don't have access to bigger institutions.”
It’s even a challenge for specialists like Dr. Ginn who wishes he had more OR time for his many patients. “I can't get cases scheduled fast enough!”
Endometriosis Awareness Month
Endometriosis Awareness Month is an annual observance that takes place during the month of March. The purpose of this month is to raise awareness about this chronic and often painful condition that affects millions of women worldwide. It is an opportunity to educate people about the symptoms of endometriosis, the challenges faced by those who live with the condition, and the importance of early diagnosis and treatment.
Or as Dr. Ginn summed it up: “This disease affects someone you know. And it is ruining her life. And it doesn't have to. There is help.”



