How MS Symptoms in Women Inform Treatments
Research Spotlight
Meet UCLA’s Dr. Rhonda Voskuhl

Rhonda Voskuhl, MD directs the UCLA Multiple Sclerosis (MS) Program. She conducts research to pinpoint treatments for neurodegenerative diseases and neurological disabilities, and has been treating patients with MS for over 25 years.
She’s an expert in how MS affects women and men differently due to how sex hormones and sex chromosomes impact the immune and central nervous systems.
“The goal of my lab is to take observations that we know are true in MS patients and try to understand them at the laboratory level to figure out why certain things happen: Why females are more susceptible than males, why males tend to do worse, and why aging is bad for MS.”
What is Multiple Sclerosis (MS)?
Multiple sclerosis (MS) is a disorder that affects the nervous system. An MS patient’s immune system attacks the nerves’ protective structures, interfering with their ability to properly send signals to the brain.
Symptoms may include, but are not limited to, paralysis, numbness, visual loss, and cognitive impairment.
Living with MS alters every aspect of a patient’s life, from their social interactions to their professional goals.
MS Symptoms in Women
MS affects women and men differently.
“Women are more susceptible to MS,” Dr. Voskuhl explains. “But when men get it, they have worse brain damage—more disability accumulation faster and at earlier ages. Womens’ symptoms tend to progress during menopause.”
Men and menopausal women have something in common: Low levels of estrogen, which plays a protective role in MS, something Dr. Voskuhl has been investigating for decades.
Her journey started in the 1990s, after she heard numerous anecdotal accounts of women with MS reporting symptom relief during pregnancy.
Since then, she’s led multiple studies that have deepened our understanding of the connection between MS and estrogen. Her lab was the first to find estrogen receptors to be protective in MS models, and that estriol, an estrogen that spikes during pregnancy, can actually be harnessed to treat MS.
A Bedside-Bench-Bedside Roadmap
Dr. Voskuhl uses a region-specific, cell-specific, and sex-specific approach to studying MS and translating findings into treatments for clinical trials.
The approach is grounded in a foundation of clinical observation.
“It’s a bedside-bench-bedside roadmap,” she explains. “After clinical observation, we go to the lab, find a new target, and do gene sequencing across the brain. We use those findings to identify a new treatment, which then goes into clinical trials.”
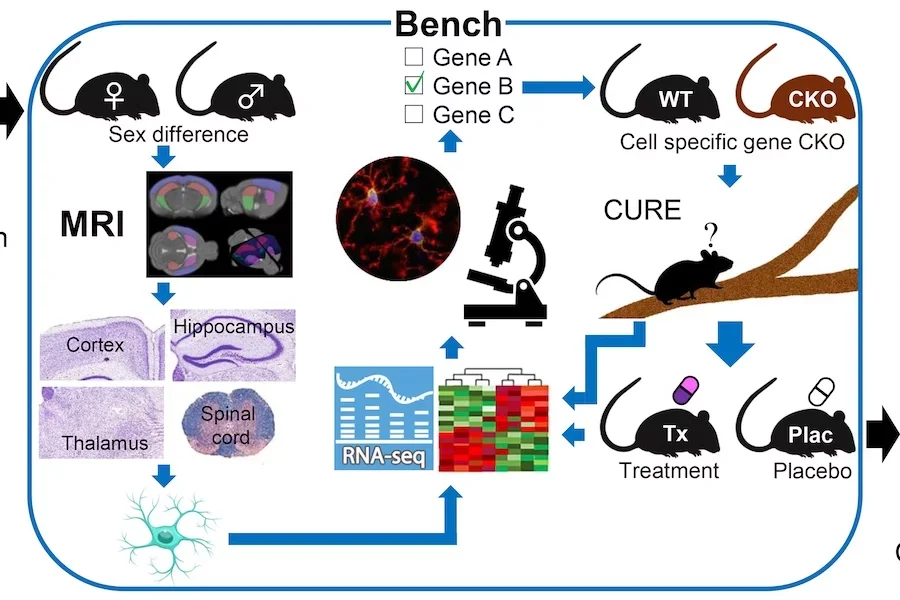
Starting with clinical observations instead of molecules, Dr. Voskuhl says, increases the odds of finding treatments relevant to MS patients.
“With molecules, you might not find anything relevant. But if you start with humans, you know something’s there. It de-risks the entire thing, so at the end, you actually have something with potential to treat people.”
Dr. Voskuhl’s roadmap also ensures more precision than a traditional bench-to-bedside model.
“This model doesn’t assume females are like males or that young people are like older people. They differ. They differ a lot in gene expression and that translates to differences in targets for different patients.”
For all the different patients suffering with different MS symptoms, this added precision can significantly improve quality of life.
About Multiple Sclerosis (MS) Awareness Month
Multiple Sclerosis (MS) Awareness Month takes place in March and was designed to help people learn about MS and how it impacts patients’ lives.



