The Different Types of Hepatitis
Research Spotlight
What Is Hepatitis? How Many Types of Hepatitis Are There?
“Hepatitis itself is a general term that refers to inflammation of the liver,” explains Dr. Yang.
There are several types of hepatitis, which are categorized as viral hepatitis and non-viral hepatitis.
The most common types of viral hepatitis are: A, B, C, D, and E.
Then there are non-viral causes of hepatitis, such as autoimmune hepatitis, alcoholic hepatitis, and drug-induced hepatitis. These forms of hepatitis are not caused by viral infections but rather by non-infectious causes such as autoimmune disorders, excessive alcohol consumption, or certain medications or toxins.
In This Article:
- Hepatitis A
- Hepatitis B
- Hepatitis C
- Hepatitis D
- Hepatitis E
- Hepatitis Symptoms
- Hepatitis Diagnosis
- Hepatitis Causes
- Hepatitis Treatment
Meet Dr. Otto Yang
Dr. Otto Yang is a prominent medical researcher and physician known for his work in the field of infectious diseases, particularly in the area of HIV/AIDS. He has been a faculty member at the David Geffen School of Medicine at UCLA since 1999 and operated a NIH-funded basic science research lab for over 25 years.
“Originally my plan was to be an oncologist but that changed when I was doing my residency training at the height of the AIDS epidemic before effective treatments were available. I was flooded with AIDS patients and seeing people dying left and right. I wanted to make a difference.”
Throughout his career, Dr. Otto Yang has made significant contributions to the understanding of HIV pathogenesis and immune responses to viral infections, most recently COVID-19. His research aims to improve treatment options for HIV-infected individuals and to shed light on the complex interactions between different viruses and the human immune system, and harnessing this knowledge for immune-based therapies relevant to viruses, cancer, and organ transplantation.
“Being able to come up with new ideas, pursue new concepts, and delve into the unknown to explore it… it's much more like play than work. So that makes my career challenging and enjoyable.”
Dr. Yang is also the Associate Chief of the Division of Infectious Diseases and Interim Director of the AIDS Institute at UCLA as well as a clinician who sees general infectious disease patients. Indeed, treating patients continually presents Dr. Yang with new challenges and finding solutions provides immense satisfaction:
“ID is the only specialty not focused on trying to change the body in terms of its structure or function. Instead we're trying to kick out foreign invaders without affecting the body. And the field of infectious diseases is very diverse and broad because the world of bacteria, viruses, and fungi is vast. Keeping up is like a continuing game of Trivial Pursuit because it’s always evolving.”
The 5 Known Types of Viral Hepatitis
“When talking about viral hepatitis, we’ve identified 5 main types that are commonly diagnosed,” says Dr. Yang. “And then there are others that are undiagnosed because we haven't identified the the causative infectious agent.”
Hepatitis A - Causes, Prevention, and Treatment
Hepatitis A is caused by the hepatitis A virus (HAV), which is typically transmitted through the ingestion of fecal matter containing the virus.
The best way to prevent hepatitis A is through vaccination. Additionally, practicing good hygiene—such as washing hands thoroughly and avoiding the consumption of contaminated food or water—can help reduce the risk of hepatitis A transmission.
In most cases, hepatitis A resolves on its own without specific treatment. The focus of treatment is primarily on supportive care to relieve symptoms and aid in recovery.
“A healthy person generally doesn't get any treatment because they they will recover. However, treatment is considered if it's a high risk patient, such as someone with a weak immune system.”
Hepatitis B - Causes, Prevention, and Treatment
Hepatitis B is caused by the hepatitis B virus (HBV), which is primarily transmitted through contact with infected blood, semen, or other bodily fluids. Additionally, an infected mother can pass the virus to her baby during childbirth: “In some parts of the world, especially the Far East, it is commonly transmitted from mother to child. Of course, that problem is starting to improve now with diagnosis and vaccinations, but it's still a significant issue.”
HBV can cause both acute and chronic infections, and chronic HBV infection can lead to liver cirrhosis or liver cancer.
The symptoms of hepatitis B can vary widely, and some individuals may not exhibit any symptoms at all. Even in chronic cases, individuals may remain asymptomatic for many years while the virus continues to damage the liver: “Because a person can be asymptomatic for decades, it's worth getting tested,” cautions Dr. Yang.

Hepatitis B can be prevented through vaccination. The hepatitis B vaccine is recommended for all infants, children, and adults who haven't been previously vaccinated. It can also be prevented by avoiding high-risk behaviors, such as engaging in unprotected sex or sharing needles.
The treatment for hepatitis B depends on whether it is an acute or chronic infection and the stage of the disease.
- Acute Hepatitis B: In most cases, acute hepatitis B does not require specific treatment. The focus is on supportive care, such as rest, proper nutrition, and staying hydrated. Monitoring liver function and regular follow-up with a healthcare provider are important.
- Chronic Hepatitis B: Antiviral medications may be prescribed to suppress the replication of the virus and reduce liver inflammation. These medications aim to slow down the progression of liver disease and prevent complications. The choice of medication and treatment duration will depend on various factors, including the patient's liver function, HBV DNA levels, and the presence of other liver conditions.
“Hepatitis B medication is very effective at keeping it in remission, although those treatments are not curative. So people need to be on treatment long term for hepatitis B.”
Hepatitis C - Causes, Prevention, and Treatment
Hepatitis C is caused by the hepatitis C virus (HCV). It is primarily transmitted through blood contact via the sharing of needles although it can also be transmitted through unsafe healthcare practices, including improper sterilization of medical equipment or accidental needlestick injuries.
“Just a few decades ago—when I was a resident—hepatitis C was called Non-A Non-B because it hadn't been identified yet and there was no way to screen for it, so it was commonly transmitted through blood transfusions,” recounts Dr. Yang. “Then HCV was discovered and now we can screen for it.”
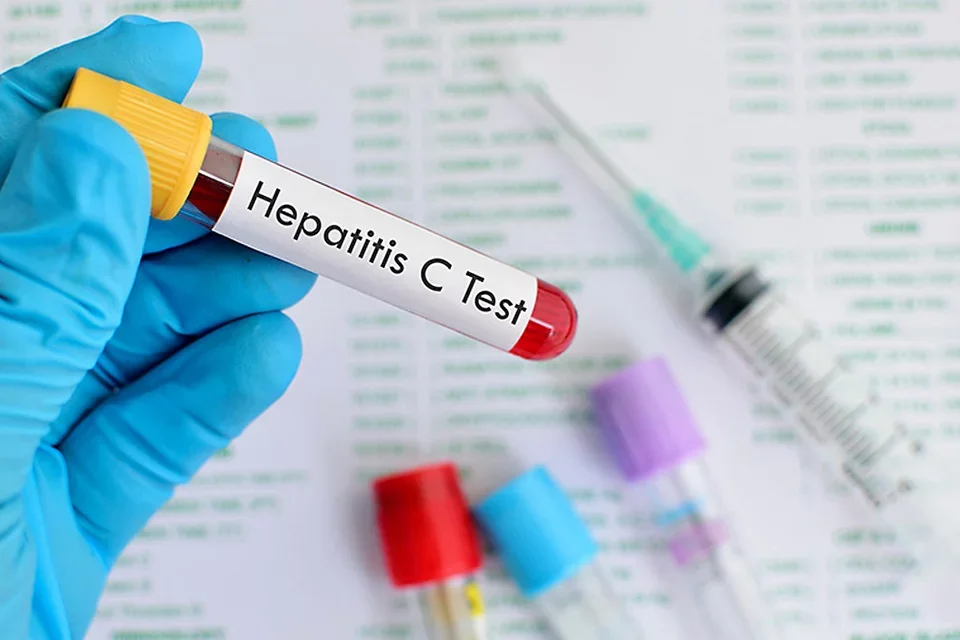
Chronic hepatitis C infection can lead to long-term liver damage, including cirrhosis, cancer, and even liver failure. It is a common cause of liver failure requiring liver transplantation. It's worth noting that symptoms of hepatitis C may not appear until the liver has already been significantly affected.
While there is no vaccine for hepatitis C, treatment for the infection has advanced significantly in recent years, thanks to the development of direct-acting antiviral (DAA) medications. “For hepatitis C, we now have medications that are curative.”
These medications specifically target the replication process of the virus and are highly effective in curing hepatitis C. The specific hepatitis C medication regimen will depend on the HCV genotype, prior treatment history, and the presence of liver cirrhosis or other underlying liver conditions.
The primary aim of hepatitis C treatment is to achieve SVR (Sustained Virologic Response), which means that the virus is no longer detectable in the blood six months after completing treatment. However—during and after treatment—regular monitoring of liver function, HCV RNA levels, and other relevant markers is important to assess treatment response and detect any potential complications.
Hepatitis D - Causes, Prevention, and Treatment
Hepatitis D—also known as delta hepatitis—is caused by the hepatitis D virus (HDV). Unlike other types of viral hepatitis, HDV cannot cause infection on its own. Also called a satellite virus, it only occurs in individuals who are already infected with the hepatitis B virus (HBV).
“The reason that a person can only get delta if they have hepatitis B is because the delta virus is defective and doesn't make its own shell. It's just a piece of genetic information, so it uses the hepatitis B shell. So that's why if you prevent hepatitis B, you'll also prevent D.”
Similar to HBV, HDV is transmitted through contact with infected blood or other bodily fluids during unprotected sexual intercourse or the sharing of needles. Additionally, an infected mother can pass both HBV and HDV to her baby during childbirth.
HDV infection can worsen the outcomes of HBV infection and increase the risk of severe liver disease. Therefore prevention is crucial for hepatitis D, and the best way to prevent HDV infection is by preventing hepatitis B infection. This can be achieved through HBV vaccination, practicing safe sex, avoiding needle sharing, and following appropriate infection control measures in healthcare settings.
The treatment for hepatitis D is primarily focused on managing the underlying hepatitis B infection, as there are no specific antiviral medications available to treat HDV directly. The treatment approach for hepatitis D includes:
- Antiviral medications used to treat hepatitis B can also help suppress the activity of HDV. These medications are aimed at reducing HBV viral replication and liver inflammation, which indirectly helps control HDV infection.
- Pegylated interferon is another treatment option for hepatitis D. It is administered as an injection and can help control HDV replication in some individuals.
- In severe cases of advanced liver disease caused by chronic hepatitis D, a liver transplant may be considered as a treatment option.
Hepatitis E - Causes, Prevention, and Treatment
Hepatitis E is caused by the hepatitis E virus (HEV). Like hepatitis A, it is primarily transmitted through the consumption of contaminated water or food, particularly in areas with inadequate sanitation and poor hygiene practices.
Prevention of hepatitis E primarily involves ensuring access to safe drinking water and practicing good hygiene and sanitation measures. In areas with a high prevalence of hepatitis E, it is advisable to drink boiled or treated water, avoid consuming raw or undercooked meat, and practice thorough hand washing before handling food.

Much like hepatitis A, a hepatitis E infection usually resolves on its own without specific treatment and most individuals recover without long-term complications:
“Clinically hepatitis A and E behave similarly in terms of their routes of transmission and outcomes. They tend to be milder and a certain percentage of people often recover spontaneously without any noticeable symptoms, especially with E.”
However in some patients hepatitis E can lead to severe complications, warns Dr. Yang: “Of course, some people are still at serious risk. For example, transplant patients whose immune systems are weak because they get drugs to prevent rejection. And pregnant women who naturally dampen their immune system, so they don't reject the baby.” In these situations, medical attention and specialized management may be necessary.
Symptoms of Hepatitis
The symptoms of hepatitis can vary in severity, and some individuals may not exhibit any symptoms at all. However, common symptoms include:
- Fatigue
- Loss of appetite
- Nausea and vomiting
- Abdominal pain or discomfort
- Pale or clay-colored stools
- Dark urine
- Jaundice (yellowing of the skin and eyes)
- Joint pain
- Fever
How Is Viral Hepatitis Diagnosed?
Even if an individual is asymptomatic, blood tests can be administered to assess liver health. Liver Function Tests (LFTs) measure the levels of liver enzymes and other substances in the blood, such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and bilirubin. Abnormal levels of these markers can indicate liver inflammation or damage.
If hepatitis is suspected, additional blood tests can detect specific antibodies (Viral Hepatitis Serologic Tests) or viral genetic material (Polymerase Chain Reaction or PCR Tests) to identify the type of viral hepatitis (A, B, C, D, or E) and determine whether it is an acute or chronic infection.
“There are 2 types of tests,” Dr. Yang explains. “One is an antibody test because if a person has antibodies that means they've been exposed. And then the other is basically direct testing for RNA or DNA, for the viral genetic material usually in the blood of the person.”

In some situations, imaging studies may be performed to evaluate the liver and assess its condition. Imaging techniques such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) can help identify liver abnormalities, such as liver enlargement, cirrhosis, or tumors.
Finally, a liver biopsy may be recommended to assess the extent of liver damage, determine the cause of hepatitis, or guide treatment decisions.
Causes of Non-Viral Hepatitis
Non-viral hepatitis refers to forms of hepatitis that are not caused by viral infections. These can be categorized into various causes, including:
- Autoimmune Hepatitis: Autoimmune hepatitis is a condition in which the body's immune system mistakenly attacks the liver cells, leading to liver inflammation and damage. The exact cause of autoimmune hepatitis is unknown, but it is believed to involve a combination of genetic and environmental factors. It predominantly affects women and often requires long-term management with immunosuppressive medications.
- Alcoholic Hepatitis: Alcoholic hepatitis is liver inflammation caused by excessive and prolonged alcohol consumption. Alcohol damages liver cells, leading to inflammation and, in severe cases, scarring of the liver (cirrhosis). It is a reversible condition if alcohol consumption is stopped, and treatment often involves abstinence from alcohol, proper nutrition, and supportive care.
- Drug-Induced Hepatitis: Certain medications, toxins, and herbal remedies can cause liver inflammation and damage. Drug-induced hepatitis can occur as an adverse reaction to medications or as a result of overdosing on certain medications. Common medications associated with drug-induced hepatitis include acetaminophen (paracetamol), nonsteroidal anti-inflammatory drugs (NSAIDs), certain antibiotics, anticonvulsants, and some herbal supplements. Treatment involves identifying and discontinuing the offending medication or toxin, along with supportive care.
- Metabolic Disorders: Certain metabolic disorders can lead to hepatic inflammation and liver damage. Examples include Wilson's disease, which is characterized by abnormal copper metabolism, and alpha-1 antitrypsin deficiency, where there is a deficiency of a protein that helps protect the liver. Treatment for metabolic disorders involves managing the underlying condition and, in some cases, specific medications or interventions.
- Ischemic Hepatitis: Ischemic hepatitis, also known as shock liver, occurs due to inadequate blood supply to the liver, typically caused by severe low blood pressure or reduced blood flow. It can be a complication of conditions such as heart failure, severe infections, or extensive surgery. Treatment involves addressing the underlying cause and providing supportive care to optimize liver function.
How is non-viral hepatitis diagnosed? Dr. Yang says it that process starts with the patient's medical history, symptoms, and risk factors, and he cites an unusual example: “An occasional cause of liver failure is poison mushrooms. So if somebody has a history of picking mushrooms, that could be the cause.”
However a liver biopsy can also prove illuminating: “During a liver biopsy, a small sample of liver tissue is obtained for microscopic examination. And the different types of hepatitis—drug-induced hepatitis versus autoimmune hepatitis versus viral hepatitis—have different appearances under the microscope.”
What Happens If Hepatitis Is Left Untreated?

If hepatitis is left untreated, it can lead to various complications and long-term health consequences. The specific outcomes depend on the type of hepatitis and whether it is acute or chronic. Potential consequences of untreated hepatitis include:
- Liver Damage: Hepatitis can cause inflammation in the liver, which, if left untreated, can progress to more severe liver damage. Chronic inflammation can lead to liver fibrosis (scarring) and cirrhosis, a condition in which healthy liver tissue is replaced by scar tissue. Cirrhosis impairs liver function and can eventually result in liver failure.
- Liver Cancer: Chronic hepatitis B or C infection, particularly if it progresses to cirrhosis, increases the risk of developing liver cancer (hepatoma). Long-term untreated hepatitis can lead to the development of liver tumors and significantly increase the risk of cancer-related complications.
- Extrahepatic Manifestations: Some types of viral hepatitis, such as hepatitis B and C, can cause extrahepatic manifestations, affecting organs and tissues outside the liver. These may include kidney problems, joint inflammation, skin disorders, or autoimmune conditions.
- Transmission to Others: Untreated hepatitis, particularly hepatitis B and C, can continue to be transmissible to other individuals. This can occur through blood contact, sexual contact, or other means of exposure, perpetuating the spread of the disease.
- Complications During Pregnancy: Pregnant women with untreated hepatitis B or C can transmit the infection to their infants during childbirth. This can lead to chronic hepatitis in the newborn, increasing the risk of liver disease and other related complications.
Dr. Yang stresses that timely diagnosis and appropriate treatment can help prevent or slow down the progression of hepatitis, reducing the risk of complications: “There are effective treatments if a person gets diagnosed, and the more severe complications—like liver cancer and liver failure—can be prevented with treatment.”
Regular monitoring, lifestyle modifications, antiviral medications, and other interventions can be effective in managing and controlling the disease. And prevention through vaccination is very safe: “There's no valid reason for vaccine hesitancy. Today the viral proteins used in the hepatitis B vaccine are actually produced in bacteria—instead of extracted from infected patients and purified—so there’s no exposure to any other human material as there was before the mid-1980s, for example.”
World Hepatitis Day
World Hepatitis Day is an annual global event observed on July 28th each year. It is an initiative of the World Health Organization (WHO) in collaboration with various governments, organizations, and individuals around the world. The main goal of World Hepatitis Day is to raise awareness about viral hepatitis, promote prevention measures, and advocate for better access to testing, treatment, and care for those affected by hepatitis.
The date, July 28th, was chosen to commemorate the birthday of Dr. Baruch Samuel Blumberg, a Nobel Prize-winning scientist who discovered the hepatitis B virus and developed a diagnostic test and vaccine for hepatitis B.



