Breast-milk pasteurizer could provide more nutritious milk for premature babies

Pasteurization process kills harmful bacteria and viruses in the milk
A UCLA Health physician has developed a portable pasteurizer that can pasteurize breast milk for preterm infants that is more economical and potentially more nutritious than milk available from donor breast milk banks.
Udayakumar Devaskar, MD, a professor of pediatrics at the David Geffen School of Medicine at UCLA, says his machine will quickly pasteurize breast milk from “super producers” — moms who produce more milk than their baby requires — to help mothers who are unable to produce enough breast milk for their premature baby.
The machine — named Kimie for a preterm infant Dr. Devaskar treated in the neonatal intensive care unit — can pasteurize up to 17 ounces at a time in about 90 minutes. A larger machine has been developed to handle greater volumes (105 ounces) of milk in one cycle and can feed roughly 20 babies per day. The pasteurization process kills all harmful bacteria and viruses in the breast milk, including HIV, cytomegalovirus (CMV) and COVID-19
“My vision is to have a smaller machine than those commercially available that is less expensive, requires less space, minimal training, and can recycle water that is used for the process,” he says. “More importantly, we can get milk from moms who have had a premature baby and it has a better composition. It’s better for premature babies than the milk we get from donor banks from moms whose baby is a couple of months old.”
At $12,000 for the smaller unit and around $15,000 for the larger unit, the Kimie pasteurizers are considerably less expensive than current pasteurizers on the market, which cost up to $60,000 and must be imported from Europe, he says.
Kimie can process breast milk in much smaller quantities than the European pasteurizers, making it convenient for use in a neonatal intensive care unit (NICU) setting, Dr. Devaskar says. And because pasteurizers are considered food devices, no approval is needed from the U.S. Food and Drug Administration, he adds.
Better than donor bank
When a mother gives birth to a preterm infant, she will not be able to produce enough milk to feed her baby for two to three days, sometimes longer, Dr. Devaskar says. Most hospitals rely on formula or breast milk from donor banks to feed such babies.
“On the other hand, in NICU there may be at least 10 women who had a baby a couple of weeks before, and their baby is still in NICU,” he explains. “They can easily make extra milk – 5, 10, 20 ccs (cubic centimeters). I can pasteurize it immediately and give it to the new baby until the natural mother’s breast milk comes in. During the interim period, premature babies need from 6 to 30 milliliters (0.20 ounce to 1 ounce) of breast milk per day.”
There are currently 31 donor breast milk banks in the U.S., two in California. The cost to purchase banked breast milk runs about $6 to $7 per ounce plus shipping, Dr. Devaskar says. Kimie, however, can process breast milk using the same technology for about $2 per ounce, he says.
Dr. Devaskar emphasizes the quality of Kimie-pasteurized breast milk is far superior to commercially available donor-bank breast milk or formula.
“Donor-bank milk is collected from moms who had a baby at full-term gestation, unlike NICU moms, whose milk has a lot more protein than milk that is collected later,” he says. “That is the main advantage.”
Why breast milk?
Dr. Devaskar likes to refer to breast milk as the “Rolls-Royce” of feeding options and points out that thousands of studies have shown its superiority to formula.
“The main reason is that mom’s milk has something like 400 different kinds of proteins, and that has a tremendous effect on the baby’s growth, including eyes, brain and everything else,” he says.
He notes that infant formula contains proteins from cows, which are different from human proteins and can result in babies making antibodies against cows’ proteins.
“Even with full-term babies, you should be using human-derived milk, as much as possible from the same mother, or if that’s not possible, from a donor mother,” Dr. Devaskar says. “Avoid using anything from the cow.”
How it works
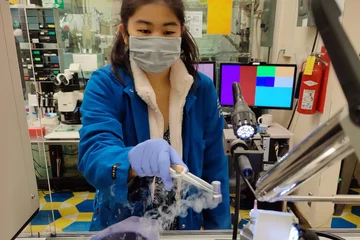
The technology behind Kimie is the same as that of the larger pasteurizers that are used in donor banks: There are two tanks – one for heating water and another for cooling it. Breast milk obtained from a donor mom is heated in the first tank to 144.5 degrees Fahrenheit. That level of heat is maintained for 30 minutes and then the milk is cooled in the second tank. The heating process kills all harmful bacteria and viruses and is then safe to give to preterm or full-term babies.
Dr. Devaskar began developing his pasteurization machine several years ago after a mother died after giving birth to a preterm baby at 27 weeks.
“There was another mother who had a baby three or four weeks earlier,” he recalls, and she had more milk than her baby required. “I realized that if I could pasteurize her milk, there would be no problem. That’s where I got the idea for this machine.”
Dr. Devaskar has an acquaintance in the dairy industry who designed a pasteurizer and sent one to the doctor. That machine proved to be too large and was not adaptable on a smaller scale. Dr. Devaskar then contacted two engineer colleagues in India who were able to design and develop a pasteurizer based on the specifications of the dairy worker’s machine with some added benefits: stainless steel cups that can be reused after sanitizing, the ability to recycle the water, and easy operation.
Kimie was put to use at centers in India and the U.S. with promising results.
While Kimie was developed with preterm infants in mind, Dr. Devaskar has discovered a multitude of situations in which his pasteurizer can be useful for full-term babies as well. They include babies who are immunodeficient; mothers who are unable to produce a sufficient quantity of breast milk to feed their baby; or mothers with a bacterial or viral infection such as COVID-19, HIV or CMV, a common virus, which, if passed to her baby through breast milk, can cause long-term health problems.
“These are mothers whose own milk can be very easily pasteurized rather than get it from a bank,” Dr. Devaskar says.
Promising results
Dr. Devaskar notes that 80% to 95% of women who deliver a baby at less than 34 weeks of gestation will be positive for the CMV antibody and will start shedding the virus through their breast milk 100% of the time. If the mother gives her raw milk to her premature baby, the baby has a 10% to 60% chance of developing CMV disease, which can be fatal, he says.
So far, Dr. Devaskar’s team has studied 60 mothers who gave birth to preterm infants and who tested positive for the CMV antibody. The mothers all fed their babies Kimie-pasteurized breast milk with no adverse reactions or complications, nor did the mothers pass the virus to their infants, Dr. Devaskar says.
Even healthy, full-term infants born to healthy moms can benefit from his pasteurization machine, he adds, as pasteurized milk can prevent gastroenteritis, asthma, dermatitis and other allergic reactions.
Dr. Devaskar’s research is being carried out with Institutional Review Board approval, and he plans to publish a study within the coming year. After that, his challenge will be to find a distributor to channel Kimie worldwide, he says.
“Every NICU all over the world should have its own machine and donor breast milk bank,” Dr. Devaskar says. “That’s my vision.”
Jennifer Karmarkar is the author of this article.