UCLA Health to test non-invasive brain stimulation treatment for chronic post-concussion symptoms

A $3 million Department of Defense grant will fund a four-year study.

UCLA Health has received a $3 million Department of Defense grant to study how non-invasive brain stimulation may improve chronic post-concussion symptoms in adults.
Short, 1- to 2-minute courses of a painless magnetic pulse have the potential to relieve symptoms of mild traumatic brain injury, said Kevin Bickart, MD, PhD, a neurologist at the UCLA BrainSPORT Program.
The four-year study starts in July 2022 and will use transcranial magnetic stimulation, or TMS, to inhibit nerve cells in the brain. TMS is currently approved by the Food and Drug Administration for some psychiatric conditions and certain types of migraine headaches.
“Having another treatment modality for chronic post-concussion symptoms at our disposal would be very exciting and could be very helpful,” said Dr. Bickart, the study’s principal investigator. “The fact that this form of TMS can be done in such a short span of time – 1 to 2 minutes -- is pretty attractive as well.”
Lingering symptoms
Dr. Bickart said that while most patients recover from mild traumatic brain injuries, including concussions, a “critical minority” experience ongoing symptoms even if there’s no observable injury on a brain scan. These include headaches, dizziness, sensitivity to light, brain fog and depression or anxiety.
Additionally, no one part of the brain is likely to be responsible for the range of symptoms.
“It can be debilitating,” he said. “The studies have shown for those people who do develop chronic symptoms, they have a harder time getting back to work, back to school or to their sport.”
Dr. Bickart said a potential cause could be a phenomenon known as fear avoidance, where patients refrain from activities or situations that could trigger symptoms. But by avoiding working at a computer, exercising, or going outside into bright sunlight, they become more sensitive to these activities instead of developing a tolerance through gradual exposure.
The study will focus on modifying a particular brain circuit that Dr. Bickart’s preliminary work shows to be overactive among people who experience ongoing symptoms. Dr. Bickart said MRIs are able to detect a blood flow pattern indicating a rigid connection between the prefrontal cortex and the amygdala.
The amygdala is a region that generates and regulates emotions. The rigidness could be indication of a maladaptation that is preventing the brain from eliminating fears and resolving symptoms.
“Certain events, activities or stimuli trigger symptoms even though they’re innocuous,” he said. “We’re hoping to extinguish that response that is not functional.”
By using TMS to disrupt the rigidity of the circuit, which would then allow for more flexibility and adaptability, the brain could readdress previously triggering situations. That could help patients reintegrate normal activities into everyday life, which would build tolerance and improve symptoms, Dr. Bickart said.
Although the research will be conducted on civilians, the findings are relevant to the military, where mild traumatic brain injury is relatively common and occurs through similar mechanisms to civilians, such as motor vehicle accidents or physical trauma.
Dr. Bickart said the study advisory board will include UCLA Operation Mend, which provides health care to post-9/11 service members, to ensure the perspective of U.S. forces are represented.
Brain scans and surveys
For the study, UCLA will recruit 90 adults with post-concussion symptoms three to 12 months after injury. Researchers will look at how brain stimulation, paired with or without an audio recording about symptom-triggering stimuli, changes the brain circuit and affects self-reported symptoms.
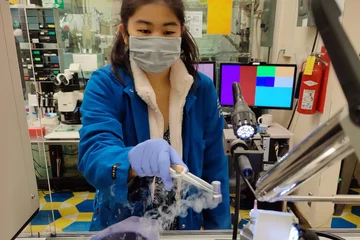
The TMS protocol uses an electromagnetic coil placed on the forehead. Patients do not require sedation and may feel muscle contractions in their forehead or eyebrow.
Dr. Bickart said the treatment will be customized to each participant by identifying the precise location of the circuit with an MRI. The area of the brain receiving stimulation is roughly the size of a quarter.
Three groups will be treated on 10 different days over the course of a month and then assessed four times by a brain MRI as well as by answering questions about their symptoms and fears of triggering them.
Participants in each of the three groups will either receive active or inactive (placebo) stimulation for 1-2 minutes while listening to self-recorded scripts about activities they fear will trigger symptoms and activities that are more neutral.
For instance, the recording might include a participant who is a student describing how when they go to a coffee shop to study, they experience brain fog. The lack of focus leads to dizziness. Next come catastrophizing thoughts that if they can’t get their work done, they’ll fail. Whereas the more neutral script might be about watching television or walking down the street.
Dr. Bickart said the idea is to see if the script will help better target the circuit that is receiving stimulation.
The participants and researchers will be blind to the type of stimulation and recording that participants receive. This will allow Dr. Bickart to figure out whether active brain stimulation plus exposure to the fear recording works better than the other possible combinations.
The first follow up for participants will happen immediately after their first treatments. Dr. Bickart said those receiving the actual stimulation, may quickly benefit.
“We expect that after a single day of treatment their MRI will look better, or show a decrease in prefrontal to amygdala connectivity,” he said.
The other assessments will be staggered over three months. Depending on further research, Dr. Bickart said brain stimulation could be expanded beyond the limited FDA-approved use.
“TMS has not bridged over to neurology as much as it probably could,” he said. “This brain specific therapy could be prescribed in clinics. People could get their TMS treatment for a month or less and potentially have multiple improvements.”
Learn more about UCLA Health neurology research.
Courtney Perkes is the author of this article.
Related:
- Taking brain cancer science from discovery to novel clinical trials
- UCLA study on migraine and sleep yields promising results for treatment
- Precision medicine meets neurology at the Clinical Neurogenomics Research Center
Original Article: UCLA Health to test non-invasive brain stimulation treatment for chronic post-concussion symptoms