Holistic approach to mental health care for people with Parkinson’s

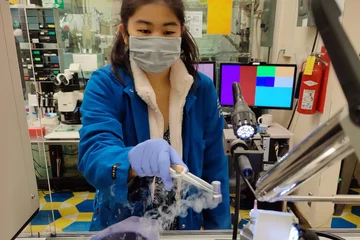
Dr. Indu Subramanian
Dr. Indu Subramanian calls for increasing disease awareness, empowering patients and community-based support
The COVID-19 pandemic has led to a heightened awareness of mental health concerns. As many people grapple with the ill effects of unrelenting stress, deep uncertainty and social isolation, structural problems in mental health care are coming to the forefront.
These issues include the stigma surrounding mental health and disparities in access to care.
For people living with Parkinson’s disease, mental health concerns too often go unacknowledged, says Dr. Indu Subramanian, neurologist at the David Geffen School of Medicine at UCLA and director of the Southwest Veteran Affairs Parkinson's Disease Research, Education and Clinical Centers.
“Part of the issue has been that mental health is highly stigmatized,” Dr. Subramanian says. “And I think COVID has shone a light on who isn't getting care.”
At the start of the pandemic, Dr. Subramanian launched a virtual support group for people with Parkinson’s disease, to help offset the negative health effects of social isolation. The group’s numbers soon swelled to hundreds of participants around the world.
Now, in an article for the journal Parkinson’s & Related Disorders, Dr. Subramanian draws on that deeply revealing experience to lay out a roadmap for a better way to manage the physical, psychological and social health of people with Parkinson's disease.
Barriers to wellness
There are numerous barriers that make it difficult for people with Parkinson’s to access adequate mental health services. For one, many clinicians lack a robust understanding of the variety of symptoms caused by the disease.
Parkinson’s disease is classified as a movement disorder because of its most visible symptoms: tremors, stiffness, difficulty walking. But there are a variety of “invisible” symptoms that can be equally devastating, including constipation, pain, sleep disruptions, and mood disorders such as depression and anxiety.
Compounding this lack of awareness is the social stigma associated with mental health care.
To break down this stigma, Dr. Subramanian says, education is critical for providers and the public. Helping patients know to anticipate these very common symptoms can help convey that it’s “normal” and expected for patients to seek mental health treatment, leading to better outcomes.
Another barrier, she says, is the misconception that the “typical” Parkinson’s patient is an older white male. “These are the pictures we see in med school,” she says. “It’s been a passion of mine to really think about who's not being served and to get their voices heard.”
Not only are doctors less likely to recognize Parkinson’s disease in people whose age, gender or race don’t fit the expected profile, such patients may find it harder to access specialist services.
Geography can be an obstacle to care as well, if patients don’t live near a large urban medical center or lack high-speed internet to access telehealth services.
Community-based resources can surmount these barriers
Dr. Indu Subramanian
A focus on wellness will be key to overcoming these issues, Dr. Subramanian says. Although “wellness” has become a popular buzzword for selling everything from spa memberships to alternative medicines of dubious efficacy, she says, when the trendy trappings are put aside, wellness remains an important core concept in medicine.
In this context, wellness refers to “the active pursuit of activities, choices and lifestyles that lead to a state of holistic health.”
In a previous study, Dr. Subramanian found that loneliness and social isolation were major risk factors for deteriorating health among people with Parkinson’s. Thus, she says, social support must be considered a central component of treatment.
A practice called “social prescribing,” in which doctors refer patients to community-based services such as support groups, yoga teachers and mindfulness coaches, has shown good outcomes in the U.K. and could be adopted more widely in the U.S., says Dr. Subramanian.
Another way to boost mental health is by arranging peer-to-peer mentoring among patients. Matching patients with a mental health “‘buddy” they regularly check in with helps patients help each other, providing an alternative to professional mental health services when these resources are scarce. It also reduces social isolation and the sense of navigating a difficult diagnosis alone.
“Just being able to say, ‘You're not alone,’ that’s huge,” says Dr. Subramanian. “That these things you’re experiencing are real, that they are part of Drthe disease; come forward and let's get you help.”
For more information, see Dr. Indu Subramanian’s blog, Parkinson Secrets, or visit the UCLA Movement Disorders Program website.