Neuroimaging in Autism
Neuroimaging in Autism
A Glimpse Into The Mysteries Of ASD

At the Brain Mapping Center on the UCLA campus, members of Dr. Mirella Dapretto's research team often meet late at night with the parents of infants. These babies, some as young as 6 weeks old, are siblings of children with autism and thus are at high risk of developing the disorder. Each baby, sleeping soundly, is bundled up and placed in an MRI scanner. Parents and researchers stand by hoping the knocking and buzzing sounds of the MRI machine coming to life won't wake the baby. If all goes well, soon researchers will be looking at specific regions of the infant's brain for clues to ASD.
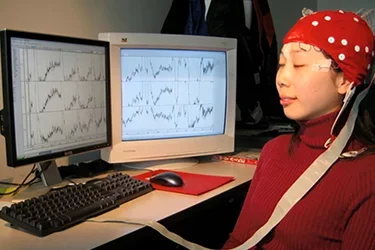
Neuroimaging is a tool that's helping rapidly to peel away some of the mystery of ASD and in the process is raising new questions and ideas about how symptoms emerge and how they may be ameliorated. Functional MRI does more than just reveal structures in the brain, such as the amygdala or the hippocampus. It also reveals brain function — what regions of the brain are involved when you're doing different things such as talking, listening, and thinking. Studies already have revealed the complexity of ASD, showing that both structure and function are involved in the disorder, sometimes in complicated and unexpected ways.
“It's as if social interaction is not intrinsically rewarding. This would explain why they may prefer to play with toys instead of looking at and engaging with people.”
Functional MRI has expanded the understanding of ASD because it's safe to use in children and infants and provides a window into what could be the earliest physiological changes — the brain architecture that gives rise to the well-known core deficits of low social engagement and hypersensitivity to the environment. A 2015 study by Dr. Dapretto, her postdoctoral fellow, Dr. Shula Green, and their colleagues, that was published in the JAMA Psychiatry magazine, found that children with ASD who are overly sensitive to sensory stimuli like noise and touch, have brains that react differently from those of their peers. Typically, developing children don’t respond as strongly to noises, visual stimulation and physical contact while children with ASD have more activity in the sensory regions of the brain.
Different Response To Sensory Stimuli
Moreover, the research showed that children with ASD seemed unable to adapt to sensory stimuli. While most people are annoyed by loud noise, such as the sound of construction in a nearby building, neurotypical children adjust to the annoyance and their brains push the noise to the background. Children with ASD seem to lack this ability to habituate; neural networks of the brain remain activated instead of gradually becoming quiet.
The researchers also found increased connectivity in the region of the brain that responds to sensory stimulation in high-risk babies compared to babies with normal risk. Moreover, the normal-risk babies showed increased connectivity in the frontal regions of brain, which are associated with attention and social interaction, when compared to the high-risk babies.

The studies in high-risk infants suggest that the abnormal brain architecture precedes the symptoms of reduced social attention and hypersensitivity to the environment. This evidence addresses a vexing question in ASD research: Which comes first: the behavior or the changes in brain's connections?
"By looking at infants at 6 weeks old, I believe you are in a better position to argue that there is some alteration in how the brain responds and is wired, and that this is playing a role in causing the symptoms that develop down the road," Dr. Dapretto says.
Neuroimaging also will play an important role in describing the variability in ASD cases, she says. Dr. Dapretto and Dr. Geschwind are collaborating on imaging genetics projects that use a functional MRI to look at the brains of children with specific genetic variance linked to increased risk for ASD. A 2013 paper examining children with the genetic risk variant on the MET gene showed differences in the way the brain is activated when looking at emotional faces as well as differences in how brain networks were connected functionally.
"By using imaging and genetic data and looking at how children behave — by putting all these measurements together — we can identify more meaningful subgroups of autism," Dr. Dapretto says. "That could be quite relevant to picking the best interventions. It's more of a precision-medicine model of autism. It also helps us understand how particular genetic risk variants may actually be influencing brain function and thus predisposing to ASD."