Hope for Pediatric Leukemia Patients
How Does Obesity Make Childhood Leukemia Harder To Cure?
Hope for Childhood Leukemia Patients

Obesity makes fighting leukemia, a devastating disease on its own, it's even harder for childhood leukemia patients. After chemotherapy, obese children with leukemia relapse 50% more often than their lean counterparts. Dr. Steven Mittelman wants to find out precisely why this happens and develop targeted interventions to save lives.
Dr. Mittelman observes the interactions of fat cells and leukemia cells to pinpoint multiple ways obesity and leukemia might interact in patients. As a physician-scientist, he also treats patients. Driven to heal as many children as possible, he leverages his clinical perspective to inform his mechanistic studies and translates his research findings into interventions that improve patient outcomes.
Obesity Worsens Cancer Outcomes
During his fellowship training in pediatric endocrinology, Dr. Mittelman attended a talk by the researcher who found that leukemia is more likely to grow back after chemotherapy in obese children than in lean children.
The finding got Dr. Mittelman's attention. He had earned a doctorate in physiology with a focus on obesity and insulin resistance, yet he had never heard about a possible link between obesity and cancer.
When I looked into the literature, there was a lot of epidemiological data showing that obese people have a much higher chance of getting cancer and dying from cancer than lean people. In fact, 20% of cancers and about 90,000 annual cancer deaths in the United States can be attributed to obesity," says Dr. Mittelman.
As Dr. Mittelman reviewed the existing research, he found a lack of investigations asking why and how cancer and obesity interconnect. Having studied whole-body physiology, Dr. Mittelman realized he had an understanding of organ and systemic interactions, which would let him tackle the cancer and obesity question from a new angle. Furthermore, he knew his clinical experience and drive to heal sick patients would strengthen his research.
"Taking care of patients gives me a perspective on the disease state and about what can and can’t be done to try to help take care of obese patients," says Dr. Mittelman.
Fat and Cancer: Cultured Together
Dr. Mittelman's lab conducts a range of translational research to understand all the possible ways fat cells and leukemia cells interact. Taking a holistic approach, the team looks beyond isolated studies of cancer cells or fat cells and observes both together in culture.
The team found that fat cells secrete a chemokine that attracts leukemia cells.
"The chemokine is likely intended to help immune cells get into bone marrow, but it also helps leukemia to enter the bone marrow," Dr. Mittelman explains.
When leukemia cells get close enough, fat cells then release amino acids and other fuels, which leukemia cells use to fuel proliferation.
When the team incorporated chemotherapies into the culture, the fat cells absorbed the drugs, metabolizing and inactivating them. As a result, many leukemia cells survived. To explain the absorption aspect, Dr. Mittelman points to fat's role in protecting the body from toxins; fat tissue absorbs toxins so they don't reach vital organs. He's not sure why fat cells might metabolize the chemotherapy drugs, but he hopes to find out in the course of his research.
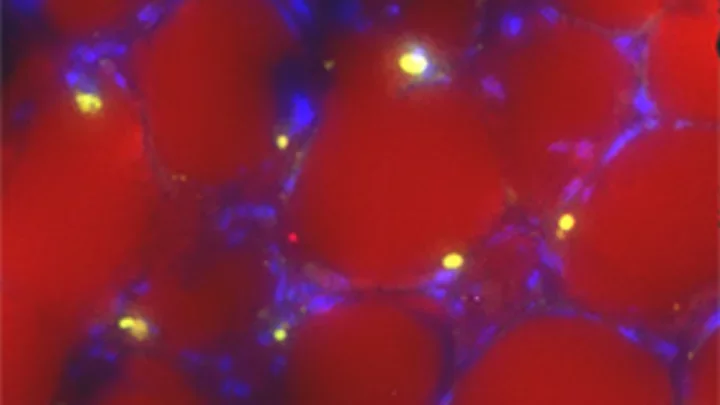
Leukemia cells infiltrate fat tissue.
Translating Research Into Interventions
Studying cell cultures elucidates many mechanistic features of the relationship between fat and cancer, but Dr. Mittelman also wants to gain relevant, translational insight from tests in preclinical models, clinical trials, and patient observations. Working closely with clinical oncologists helps Dr. Mittelman ensure that his findings are relevant to patients with leukemia.
Dr. Mittelman's patient observations reveal that obesity makes childhood leukemia treatment less effective within the first month of chemotherapy. Compounding the treatment inhibition, children with leukemia tend to gain fat tissue during their first month of treatment as a result of steroid intake and a general decrease in wellness.
Looking for a way to help these kids, the team conducted tests on preclinical animal models. In these models, diets initiated before chemotherapy greatly improved leukemia survival rates.
To find out if the promising results had relevance for humans, the team needed to test diet and exercise interventions in a clinical trial. Dr. Mittelman's lab became the lead study laboratory on the Improving Diet and Exercise in Acute Lymphoblastic Leukemia (IDEAL Weight in ALL) trial, conducted by Principal Investigator, Dr. Etan Orgel. The trial tests the effect of a modest diet and exercise increase on childhood leukemia patients.
"It's too early to say if it has significant effects or not, but I can’t wait to find out," says Dr. Mittelman.
Enhanced Treatments for Obese Cancer Patients
Many of Dr. Mittelman's findings on the interactions between fat cells and leukemia cells could have relevance not just in leukemia treatments, but also in treatments of other cancers where obese patients typically have worse outcomes, including breast cancer, colon cancer, and prostate cancer. Furthermore, treatments for other cancers incorporate the chemotherapies Dr. Mittelman has seen fat cells absorb, so his research might also extend to enhancing those therapies.
There are a lot of cancers where obese patients have a worse outcome, so it could be that once we find these mechanisms, we’ll be able to go back and see that this also explains part of what’s going on with other cancers," Dr. Mittelman says.
Knowing he has support from UCLA as a whole and within the Metabolism Research Theme, Dr. Mittelman believes he'll be able to answer the mountains of questions standing between him and a complete understanding of the relationship between leukemia and obesity.
"There are so many smart people here at UCLA doing so many different things. When you need a partner to help you with something, you can find at least ten people who are experts in that specific field," says Dr. Mittelman.
When Dr. Mittelman has a question about how metabolism works on a cellular level, a number of colleagues can provide detailed answers. When he needs specialized equipment to take a specific measurement, someone can help him get access. Through these collaborations, Dr. Mittelman knows he'll find ways to extend and streamline his research, and ultimately, save lives.