Autism Biomarkers
The Development of Autism Biomarkers
The Biomarker Challenge
Since ASD is a heterogeneous disorder, no one autism treatment will benefit all children. But in most places of the country, an ASD diagnosis is based on whether a child meets the criteria for the disorder based on a list of symptoms; treatment typically depends on a family's financial resources and whatever programs or therapies happen to be available in a community.
Diagnosing ASD isn't as easy as taking a blood sample, conducting a brain scan or measuring the circumference of a child's head. One of the more challenging aspects of research and treatment is the lack of objective biological measures to diagnose the condition or precisely measure improvements in a child receiving treatment.
"The autism diagnosis is based on a list of behaviors that emerge during early development," says Dr. Jeste. “As you can imagine, there can be quite a bit of variability in the ways these behaviors present. There's a saying in our field that if you've met one child with autism . . . you've met one child with autism, meaning that generalization about the condition is challenging."
Informed by the genetics, researchers at UCLA are working to identify brain-based biomarkers that may precede an ASD diagnosis and that might help place children with ASD into meaningful subgroups. Identifying bio

markers can inform more targeted treatments, assist researchers in monitoring the effect of various therapies and even provide clues regarding the molecular processes involved in the disorder.
"Treatments will only work if we understand exactly what we are treating and if we can understand which treatments will work for which kids," Dr. Jeste says. "Research in brain-based biomarkers can help us accomplish this goal."
“ ”
Old Tech With Promising New Tricks
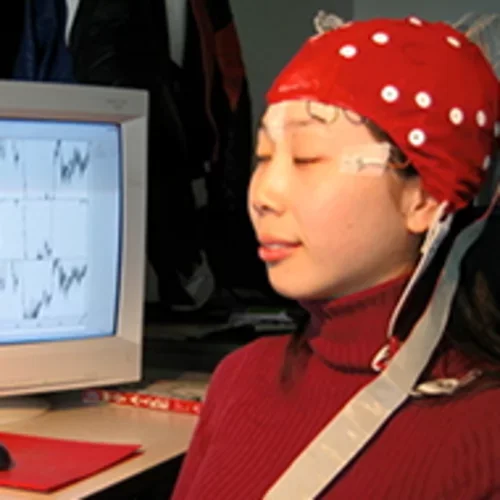
One promising tool in the study of brain-based biomarkers in ASD is electroencephalography, or EEG. Invented almost 90 years ago, EEG is a noninvasive and safe test used to detect the firing of neurons in the brain. The firing of neurons generates an electrical signal that can be measured at the scalp. To record EEG, electrodes are attached to the scalp, and brain wave patterns are safely and painlessly recorded. The technology has been refined and computerized and is proving to be an eye into the brains of young children with ASD who are at high risk of developing the disorder.
"EEG is basically examining the activity of the brain in real time," says Dr. Jeste, who is an expert in EEG use in ASD research and joined UCLA in 2010 to establish an electrophysiology program in the autism center, now known as the developmental neurophysiology lab. "We should be able to use EEG to start understanding different processing patterns in high-risk infants and in children with autism across the spectrum. If you can give a baby a task or show them pictures while recording EEG, you can get a readout of how the brain is processing information without having to ask the infant or child to provide an answer. You also can measure the way in which brain networks are connected and functioning. That's pretty powerful."
Biomarkers are proving especially useful in identifying babies at high risk for developing ASD (either because they have a sibling with the disorder or are showing some early symptoms, such as not engaging with caregivers. Physiological measures, such as EEG, magnetic resonance imaging (MRI) or eye tracking, are now used in almost all of UCLA's studies in high-risk children.
Several studies comparing children with ASD or those at high risk to normally developing children have revealed differences in brain function. Scientists even can begin to parse out certain subgroups of children who have particular patterns of abnormal neural connections. These subgroups may be linked with specific genetic causes.
ASD Biomarkers for earlier intervention
Biomarker studies open the door to earlier intervention, Dr. Jeste says. Research over the last two decades has revealed that intensive early therapy can help children with ASD overcome some of the core deficits of the disorder and maximize their developmental outcomes. Today, some children who receive early, intensive therapy are even able to enroll in mainstream kindergarten classes. This progress is evidence of the brain's neuroplasticity early in life and its ability to change, develop and compensate for deficits.
Studies have already begun to identify some biomarker patterns that can distinguish high-risk and low-risk children. Biomarkers are also emerging as potential tools to assess how treatment is working. One study involves children with tubercular sclerosis complex, a genetic disorder that is diagnosed early in life. These children have a high risk of also developing ASD. Prior studies from Dr. Jeste at UCLA and colleagues at Boston Children's Hospital found that reliable behavioral and EEG predictors of ASD could be measured by 12 months of age. Based on that finding, Dr. Jeste and Dr. Kasari recently began an early intervention study that targets social communication skills as early as 12 months of age in these infants. The investigators are using brain imaging and EEG to assess the children as they develop.
- How early can we intervene to improve development in these high-risk infants?
- What are the mechanisms that affect change?
- How can we better understand why are some children are making changes and other kids are not?
Biomarkers might also prove valuable to help predict which children will respond to specific therapies. For example, there is a broad range in language skills among children with ASD. "We want to know if we can predict, based on the biomarkers, who will make gains," Dr. Jeste says. "Sometimes this prediction is challenging to do through behavioral testing alone. Studying the brain gives us a much more refined view of what is actually happening."
Improving the methodology of testing for ASD
As a leader in the development of biomarkers for ASD research and treatment, UCLA also is investing considerable time and effort to improve the methodology of testing. As biomarker use increases and eventually spreads into clinical practice, doctors and therapists will require assistance on appropriate use of the technology.
A recently funded, five-site project called the Autism Biomarker Consortium for Clinical Trials has begun to help develop testing standards and to identify robust biomarkers in children with ASD. The project, led by Dr. James McPartland at Yale University with Dr. Jeste serving as principal investigator at UCLA, has garnered one of the largest NIH grants given to a single ASD study.
In the future, Dr. Jeste says, researchers hope to improve the technology so much that the 128-electrode EEG used in research can be restructured into a simpler system with fewer electrodes that a pediatrician can perform in an office setting.
Biomarker research represents a strong scientific approach not only to understanding the underlying neurobiology of ASD but also to improve diagnosis and treatment monitoring — an approach that UCLA researchers hope will drive public opinion and education about the disorder. The field has been stymied at times by a contingent of professionals and parents who contend that the disorder is not genetic but is caused by environmental factors, such as vaccines administered in early childhood.
Project Spotlight
Autism Biomarkers Consortium for Clinical Trials is a multicenter research study based at Yale that spans some of the nations best medical research centers.
Our knowledge about early brain development in ASD, as evidenced by the imaging and EEG research being performed at UCLA and nationwide, can help debunk the vaccine myth. Evidence of changes in neural processes, such as brain connectivity as early as three months of age, can help address some harmful misperceptions. "It is our job, as a scientific community, to share with the community our discoveries and insights in a way that will help them make more informed decisions," Dr. Jeste says. "The research being done at UCLA gives us a lot of hope that scientific advances will ultimately maximize a child’s potential for healthy development."



