UCLA clinical trial tests anti-inflammatory drug to improve outcomes in patients with COVID-19 and heart damage
A new UCLA clinical trial, COLHEART-19, is testing a currently available anti-inflammatory drug to treat heart damage associated with COVID-19.
The phase two clinical trial will assess if colchicine – a widely available anti-inflammatory drug that has long been used to treat gout – can reduce inflammation and thereby improve short-term outcomes in patients hospitalized with COVID-19 who also show evidence of heart damage.
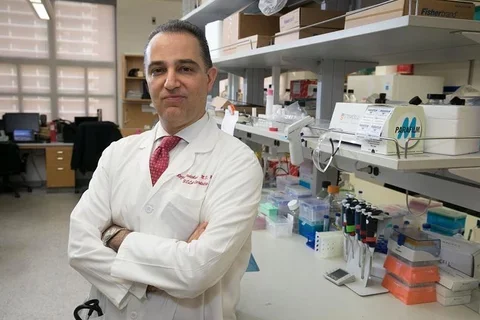
Dr. Reza Ardehali, associate professor of cardiology at the David Geffen School of Medicine at UCLA and member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research, is leading the trial in collaboration with UCLA cardiologists Dr. Amir Rabbani, Dr. Rushi Parikh and Dr. Asim Rafique. The trial is receiving substantial support from the UCLA Clinical and Translational Science Institute and the David Geffen School of Medicine.
“To date, treatments available for COVID-19 remain limited as randomized controlled trials have failed to identify effective therapies,” said Parikh, an assistant clinical professor of cardiology. “Colchicine, given its well-established safety profile, widespread availability, and relatively low cost, would represent a pivotal shift in the management of COVID-19 associated heart damage.”
Up to 80% of patients infected with SARS-CoV-2, the virus that causes COVID-19, experience mild symptoms that resolve on their own. However, patients who develop more severe symptoms can experience difficulty breathing, lung injury, heart damage and kidney failure.
A study published in the Journal of the American Medical Association found that of up to one in five patients hospitalized with COVID-19 in Wuhan, China ended up with heart damage. Furthermore, heart damage was strongly linked with poor outcomes. The death rate for patients with heart damage was 51% while the death rate for those without heart damage was 4.5%.
Patients who had heart disease prior to infection were more likely to show heart damage after COVID-19 infection. However, some patients with no previous heart disease also showed COVID-19-associated heart damage
Severe cases of viral infection are known to cause myocarditis, which is a massive inflammatory response in the heart. This inflammation weakens the heart, creates scar tissue and limits the heart’s ability to pump blood. Myocarditis can lead to heart failure, abnormal heartbeat and sudden death.
COVID-19 infection is suspected to cause heart inflammation in a number of ways. Whether this process resembles the myocarditis seen with other viral infections is not yet clear. The most serious source of damage is a cytokine storm, which can occur when the body’s normal immune response causes excess inflammation that destroys healthy tissue and injures organs such as the heart, liver and kidneys. In COVID-19 patients, cytokine storms have been linked with severe multi-organ failure including irreversible damage to the heart.
In multiple trials, colchicine has been shown to reduce inflammation in the heart and improve outcomes following open heart surgery and heart attack. Ardehali and his collaborators suspect that when given to patients early on in their hospitalization for COVID-19, colchicine could lower excessive inflammation and reduce damage to the heart.
“We’ve never faced anything like COVID-19, however we have had experience treating patients who have inflammation of the heart,” said Ardehali, who is also a professor of molecular, cellular and integrative physiology and an associate chief of cardiology in regenerative medicine. “Colchicine has been very effective in treating patients who have inflammation of the heart so we’re putting two and two together: if there is inflammation in the heart that causes damage after COVID-19 infection, perhaps this medication could help.”
The trial has received approval from the Food and Drug Administration to begin enrolling patients at UCLA Ronald Reagan Medical Center and UCLA Santa Monica Hospital.
Patients are eligible to enroll in the clinical trial if they have confirmed COVID-19, are admitted to the hospital and have any evidence of heart damage. In order to determine if colchicine is beneficial, half of participating patients will be randomized to receive standard of care treatment plus colchicine twice daily for 30 days, and half of the patients will receive standard of care treatment without colchicine.
“Colchicine – if proven effective – has other advantages,” said Rafique, who is an assistant clinical professor of cardiology. “It is available in pill form and can be safely taken at home unlike other COVID-19 anti-inflammatory treatments, which require IV administration and closer monitoring in the hospital.”
Patients will have blood tests and an ultrasound of the heart at the beginning of the study and at one month after enrollment. Investigators will call patients at three months to gather outcomes. This will enable the researchers to determine if colchicine improves short-term clinical outcomes in hospitalized COVID-19 patients.
“Our trial is unique in that we focus on the cardiovascular effects of the disease process,” said Rabbani, an assistant clinical professor of cardiology. “While public awareness of the often-serious cardiac complications of COVID-19 has risen, there are few randomized, controlled trials aimed at understanding how best to treat those complications in an effective way.”
To learn more about this clinical trial, visit its page at clinicaltrials.gov. If you think you might be eligible to enroll, please contact the study coordinator, Danielle Campbell, at DMCambell@mednet.ucla.edu.
Original Article: "UCLA clinical trial tests anti-inflammatory drug to improve outcomes in patients with COVID-19 and heart damage"



