Immunotherapy drug combo helps extend the lives of metastatic melanoma patients
Combining two immune checkpoint inhibitors helps overcome resistance
A research team co-led by UCLA investigators has shown that an immunotherapy drug combination can be an effective second-line therapy for patients with an aggressive and deadly type of melanoma that is resistant to the widely used immunotherapy drugs known as PD-1 inhibitors.
In clinical trials, the investigators found that the combination therapy could extend the amount of time patients live without their cancer worsening, known as progression-free survival, and that it helps overcome their resistance to prior immunotherapies — which would allow more people to benefit from the treatment.
The approach combines the immunotherapy drugs ipilimumab and nivolumab, a combination that not only showed a longer progression-free survival, but also a greater overall response rate to treatment compared to those who received the current standard therapy of ipilimumab alone.
The multicenter clinical trial was conducted by the SWOG Cancer Research Network, a group funded by the National Cancer Institute; the findings were reported in the journal Nature Medicine.
“The results are practice-changing,” said Dr. Antoni Ribas, the study’s senior author, a professor of medicine at the David Geffen School of Medicine at UCLA and director of the UCLA Health Jonsson Comprehensive Cancer Center’s Tumor Immunology Program. “The combination approach should be the preferred drug regimen for people with cancer that has not responded to prior immunotherapy treatment.”
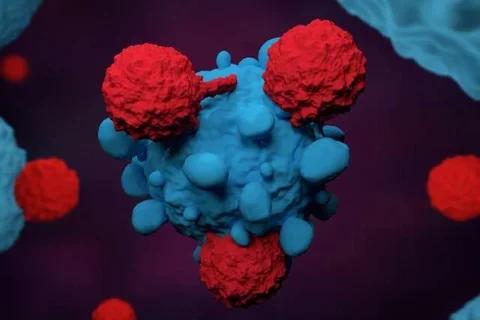
Both ipilimumab and nivolumab are immune checkpoint inhibitors that work by blocking proteins in the body that can prevent the immune system from attacking cancer cells. Nivolumab, also known as a PD-1 inhibitor, blocks an immune checkpoint protein on T cells called PD-1. Ipilimumab, also known as a CTLA-4 inhibitor, blocks the protein CTLA-4. These inhibitors can help restore the natural ability of T cells to attack cancer cells.
Currently, patients with advanced metastatic melanoma are treated with PD-1 inhibitors as a first-line defense. While these checkpoint inhibitors have been a significant advancement for treating people with a variety of advanced cancers, more than 50% of metastatic melanoma tumors are resistant to the drug. When resistance occurs, patients are often switched to CTLA-4 inhibitors.
Before this study, it was unclear whether patients whose cancers are resistant to the PD-1 inhibitors can continue the PD-1 agent in combination with a CTLA-4 inhibitor or if they should be switched to a CTLA-4 inhibitor alone.
“The combination had the potential to better activate the immune system against cancer by simultaneously blocking two main immune checkpoints, increase the immune infiltration in the cancer and thereby overcome resistance to anti-PD-1 alone,” said Ribas, who is also a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research.
To see if a combination approach was more effective than using CTLA-4 inhibitors alone as a second-line therapy, researchers enrolled 91 patients in the multicenter clinical trial who had already been treated with an anti-PD-1 immunotherapy drug and had not received an anti-CTLA-4 drug. All of the patients enrolled had cancer that had not responded to the current therapy. Sixty-eight patients were randomly assigned them to receive the combination of ipilimumab and nivolumab and 23 patients received just ipilimumab.
The team of investigators measured progression-free survival as the main endpoint and also looked at other factors like how well the immune cells were infiltrating the tumors, how the cancer responded to the treatment, how long patients lived and side effects.
The team found the participants receiving combination therapy had a 37% improvement in progression-free survival compared to participants who received ipilimumab alone. Patients receiving the combination treatment also had higher response rates, with 28% of patients seeing their tumor shrinking compared to only 9% of those who received ipilimumab alone.
Side effects were similar to what was previously known about this combination of drugs, with the most frequent severe adverse event being diarrhea, which happened at the same rate with ipilimumab alone or in combination.
“We found approximately one third of the patients receiving the immunotherapy combination had improved outcomes,” Ribas said. “Sequencing immunotherapy treatments as was tested in this study is the next step forward in our efforts to better tailor the treatment options while limiting exposure to side effects. Patients with advanced melanoma can get an anti-PD-1 treatment upfront and only add the anti-CTLA-4 ipilimumab if they do not respond, so only the patients that need the combination are exposed to the increased toxicities.”
The study was funded by grants from SWOG, National Institutes of Health and the National Cancer Institute.
Ari VanderWalde, MD, MPH, an investigator with West Cancer Center and Research Institute in Germantown, TN is the first author of the study and SWOG study chair.
Other UCLA authors include Katie Campbell, Dr. Phillip Scumpia, Dr. Lawrence Kuklinski, Dr. Bartosz Chmielowski, Egmidio Medina, Cynthia Gonzalez, Ignacio Baselga-Carretero, Agustin Vega-Crespo and Ivan Perez Garcilazo.
Photo credit: iStockphoto
Original Article: Immunotherapy drug combo helps extend the lives of patients with metastatic melanoma



